Causes of pancreatitis

Pancreatitis Pancreatitis; from pancreas, pancreas is inflammation of the pancreas. It may present with upper abdominal pain, bloating, unreasonable weight loss, indomitable vomiting, and steatorrhea, in which stool is poorly flushed from the toilet and appears fatty in appearance.
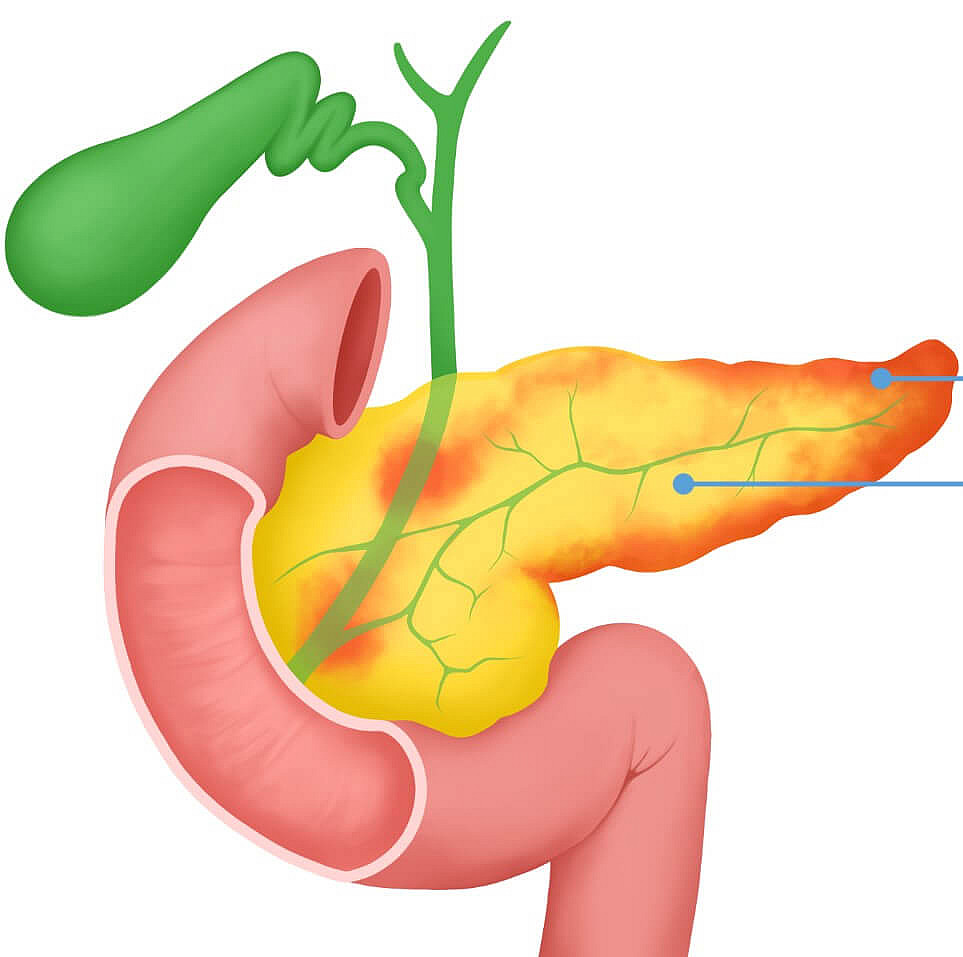
Pancreatitis is an inflammatory disease of the pancreas that can affect nearby tissues. The main symptoms include upper abdominal pain due to malfunction of the pancreas. This function involves the production of digestive enzymes and hormones.
The pancreas fulfills two key tasks:
The exocrine function is the production and release into the duodenum of enzymes such as trypsin, protease, amylase, and lipase. These enzymes are essential for digestive breakdown of proteins, carbohydrates, and fats.
Endocrine function related to the synthesis of insulin and glucagon hormones. These hormones regulate the level of sugar (glucose) in the blood and help keep it stable.
The lack of digestive enzymes leads to frequent digestive disorders, and nutritional deficiencies may develop if pancreatitis is prolonged.
The impaired hormone production in turn causes changes in carbohydrate metabolism, which can lead to diabetes mellitus.
Causes of Pancreatitis
Major factors that contribute to pancreatitis include alcohol abuse, smoking, and cholelithiasis.
Excessive alcohol consumption increases the viscosity of pancreatic juice, leading to blockage of pancreatic ducts. This makes the drainage of juice difficult and increases the pressure inside the ducts. The active enzymes, when accumulated, begin to destroy gland tissue, causing inflammation. Ethanol metabolites also directly damage pancreatic cells.
Smoking causes vascular spasm that impairs the blood supply to the pancreas and worsens its damage.
To understand the relationship between pancreatitis and gallstone disease, it is important to know that the pancreas and gallbladder have common ducts that connect and open into the duodenum. In biliary colic, the stone exiting the gallbladder may block the connection. As a result, bile and pancreatic juice return to the pancreas under high pressure, causing injury and inflammation and tissue necrosis.
Signs of pancreatitis
Severe pain in the upper abdomen (near the navel, subcostals). Pain may be localized or radiated to the back. It increases after meals, when people suddenly move, cough, or breathe deeply, and decreases when people sit or lean forward.
Nausea and frequent vomiting, which usually do not bring relief.
Excessive salivation, burping with air, or eating.
Lack of appetite and aversion to oily food.
Diarrhea (diarrhea), which causes a large amount of foul-smelling, mush-like stool that has a fatty sheen and pieces of undigested food.
Flatulence (bloating).
Fever in the body.
Jaundice is a yellowish discoloration of the skin and whites of the eyes and mucous membranes.
Weight loss due to decreased appetite or excessive dietary restrictions
General weakness and fatigue.
Diagnosis of Pancreatitis
In addition to medical examination, laboratory and instrumental diagnostics are performed to establish the diagnosis of "Acute pancreatitis" or "Chronic pancreatitis".
Laboratory tests include tests of blood, urine, and stool.
A complete blood count (complete blood count) is done to check for signs of inflammation.

Instrumental methods of diagnosis of pancreatitis:
Ultrasound examination (ultrasound) of the abdominal organs. It can detect signs of acute pancreatitis, such as an enlarged pancreas, fuzzy contours, free fluid in the abdomen and omentum, and other characteristic changes.
Computed tomography (CT) or magnetic resonance imaging (MRI) of the abdominal organs These techniques can be used to assess severity and refine the diagnosis, particularly if conservative treatment is ineffective. MRI is preferred, but sometimes CT is indicated if contraindications (eg, metal implants) are present or unavailable.
Endoscopic ultrasound (endo ultrasound). Doctors suspect stones in the ducts of the pancreas, especially if there is biliary pancreatitis.
Laparoscopy. This method is used if no definitive diagnosis can be made by other instrumental studies. Laparoscopy can provide a visual view of the abdominal organs and additional procedures as needed.
Treatment of Pancreatitis
Treatment of pancreatitis may be conservative or surgical, depending on the severity of the disease.
In acute pancreatitis, the person is hospitalized immediately in the surgical ward. The main treatments include
Starvation: The person is not allowed to eat anything for 24 hours to reduce the burden on the pancreas.
Infusion therapy: Intravenous fluids to maintain fluid and electrolyte balance and eliminate toxins.
Drug treatment: Prescribe drugs that reduce smooth muscle tone and the production of hydrochloric acid to reduce inflammation and pain.
A complex of peptide compounds, these peptides promote the restoration of normal metabolism in cells and support the optimal functioning of the pancreas.

