Pain in the mouth (stomatitis)

Stomatitis, sores in the mouth is a generalized name for a group of diseases that are characterized by inflammation of the oral mucosa (ORS). Dentists are most common among children, but in adults, they may be chronic or a symptom of various disorders such as internal disorders or metabolic disorders.
Symptoms Pain in the mouth
Stomatitis manifestations depend on the specific form. In clinical practice, there are several types of stomatitis, which differ in their causes. Despite the variety of forms, there are common symptoms common to all types:
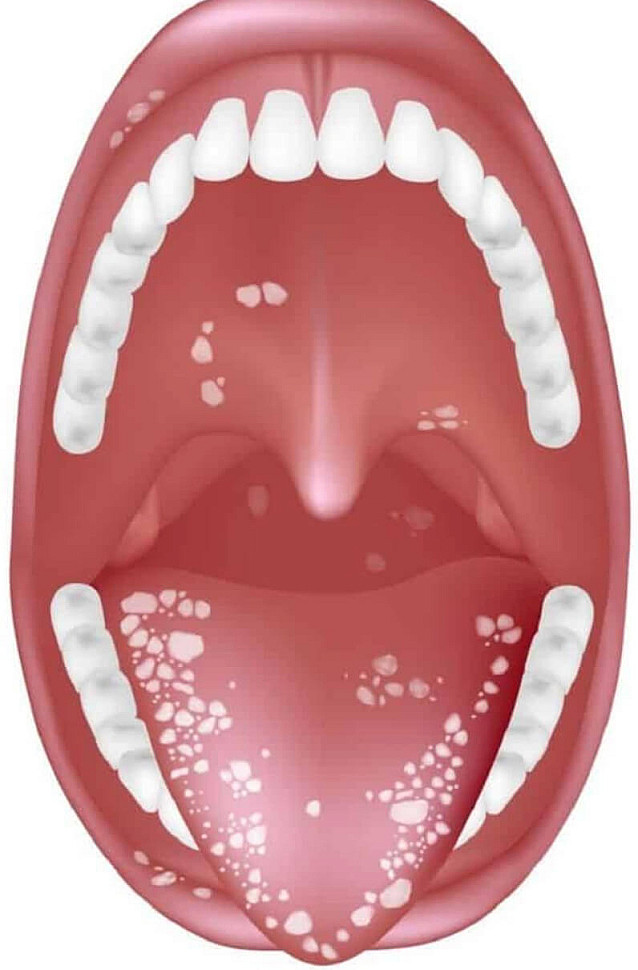
Redness, erosion, and sores (aphthae) on the lining of the mouth, such as those on the inside of the cheeks, lips, floor of the mouth, or gums.
Lesions that may appear as spots, blisters, ulcers, or patches of different density and color.
Pain is felt when erosions and sores are exposed and increase when people eat, drink, or talk.
In severe cases, a general feeling of illness, fever, symptoms of intoxication, and other signs may occur.
Causes of Stomatitis Pain in the mouth
Stomatitis can occur for a variety of reasons. One of the most common is the herpes virus, which by the age of 16 infects about 96-98% of the population. After infection, the virus may remain inactive for a long time, but under exposure to triggers, it activates and causes clinical symptoms. Such factors include injuries, weakened immunity, and others.
Another cause of stomatitis may be yeast-like fungi that are part of the oral microbiome and are activated under certain conditions. It can occur while taking medication or having poor oral hygiene. If candidal stomatitis cannot be treated, doctors recommend that people be evaluated to rule out disorders such as diabetes, immunodeficiency, and others.
Factors that contribute to Pain in the mouth:
- Childhood;
- decreased salivation (xerostomia);
- changes in the composition and properties of saliva;
- smoking;
- diseases of internal organs;
- Inadequate oral hygiene
- using dentures;
- caries;
- gum diseases;
- chemotherapy and radiation therapy for cancer.
The exact causes of some types of stomatitis, such as chronic recurrent aphthous stomatitis, are not fully understood. However, there is speculation that its development may be related to diseases of the internal organs and allergic reactions. Some experts believe that aphthous stomatitis may be an early sign of gluten intolerance, but this hypothesis has not yet been supported by sufficient evidence.
In adults, chronic injury, such as wearing improper dentures, is a common cause of stomatitis and causes irritation of the oral mucosa.
Dentistry includes analysis of complaints, visual inspection, and additional tests to identify the cause of inflammation. Stomatitis can be a manifestation of diseases of the internal organs. In most cases, a visual examination and complaint collection are sufficient for diagnosis. A dentist evaluates the mucosa of the mouth, the presence of erosions, aphtha and other changes. Doctors of other specialties can take part in the process of diagnosis and treatment: gastroenterologists, endocrinologists, allergologists and others.
Laboratory tests may be needed to identify the organism:
Smear the mouth to exclude or confirm fungi or bacteria.
Blood tests to detect infectious diseases
Treatment of stomatitis depends on the cause and on additional factors such as age and oral status. Etiotropic therapy includes appropriate drugs, including topical drugs. Viral stomatitis is treated with antiviral agents, bacterial antibiotics, candidal antifungal agents, etc. Treatment of recurrent aphthous and allergic stomatitis is more difficult and requires the involvement of specialists of different profiles. The main task is to eliminate the factors that provoke stomatitis.
When treating stomatitis, you should observe the following rules Pain in the mouth:
Carefully observe oral hygiene.
After the symptoms disappear, change the toothbrush, regardless of its duration.
Eliminate sweet, spicy, sour and other products that irritate the mucous membrane.
Follow hygiene practices to prevent spread of infection to family members.
Some forms of stomatitis, such as severe herpetic stomatitis, can cause fever above 39° C, delirium, and an inability to eat or drink. Treatment of these forms is carried out in hospital under the supervision of doctors. Toxic symptoms may be serious in severe stomatitis.
Prevention of stomatitis: key recommendations
Stomatitis prevention involves several important steps to keep the mouth healthy and prevent inflammation.
Careful oral hygiene is the foundation of prevention. Regular brushing, flossing and rinsing, and adherence to a dentist's recommendations help keep the gums healthy and prevent bacteria from accumulating. In December 2010, a study was published confirming that good oral hygiene facilitates easier treatment of stomatitis and reduces the risk of recurrence.
Regular visits to the dentist are also important to prevent stomatitis. Preventive examinations identify and correct potential problems early, such as caries, defects in seals, crowns, and dentures. It is particularly important to prevent allergic stomatitis, which may be caused by a reaction to dental materials. In 2017, the journal described cases of allergic stomatitis caused by the use of adhesives in dentistry, including materials for braces.

