Pancreatitis and Smoking

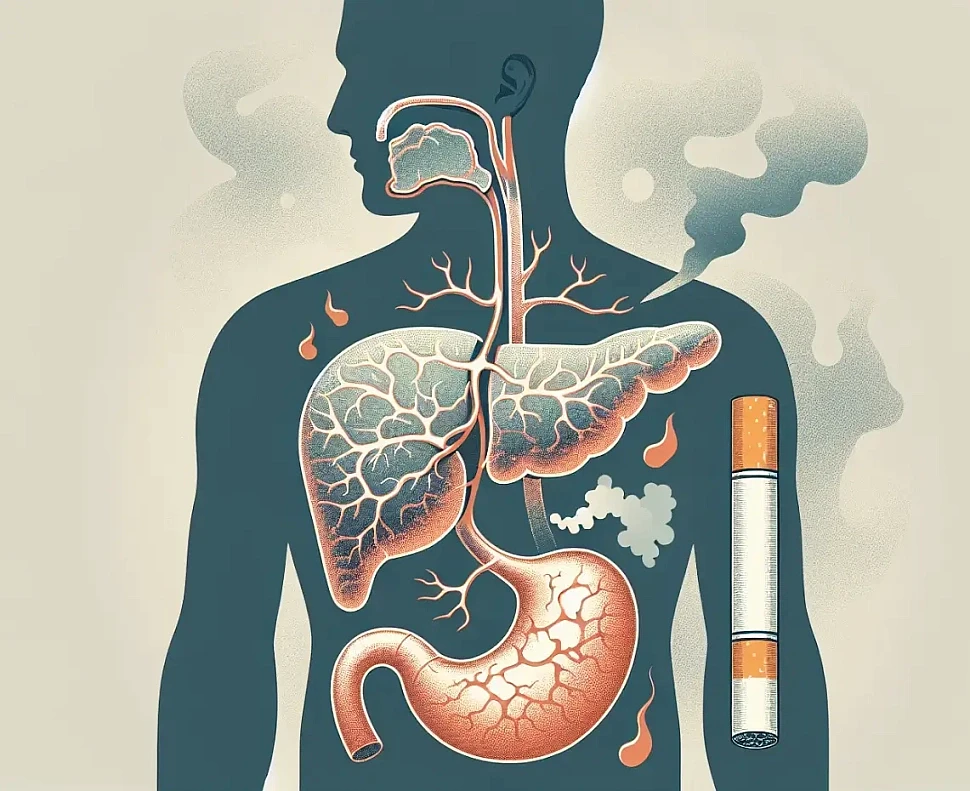
Most people associate smoking with lung problems or heart disease, but few realize how strongly it affects the pancreas — one of the most sensitive and vital organs in the body. The pancreas plays a key role in digestion and blood sugar regulation, yet it’s also one of the first organs to suffer silently from lifestyle choices such as smoking.
Recent research in both the United States and the United Kingdom has shown a clear and alarming connection between smoking and pancreatitis — a painful and sometimes life-threatening inflammation of the pancreas. Whether you’re a casual smoker or have been smoking for years, understanding this link could make a major difference to your health.
How Smoking Affects the Pancreas
Cigarette smoke contains more than 7,000 chemicals — including nicotine, carbon monoxide, formaldehyde, and various heavy metals. When these toxins enter the bloodstream, they reach the pancreas quickly and begin to interfere with its delicate tissue structure.
Nicotine reduces blood flow to the pancreas, depriving it of oxygen and essential nutrients. Over time, this leads to tissue damage and inflammation. Toxic compounds also trigger oxidative stress, which increases the production of harmful molecules that attack pancreatic cells.
But the damage doesn’t stop there. Smoking disrupts the way pancreatic enzymes are produced and released. Instead of moving safely into the digestive tract, these enzymes can become trapped within the organ, essentially causing it to “digest itself.” This process is one of the main triggers of acute and chronic pancreatitis.
Smoking and the Risk of Pancreatitis
Several studies from major universities, including Harvard and Oxford, have confirmed that smokers are significantly more likely to develop pancreatitis than non-smokers.
Smokers are 2–3 times more likely to experience chronic pancreatitis.
The risk increases even more for those who combine smoking and alcohol consumption, as both damage pancreatic cells in different but complementary ways.
Even light or “social” smoking can raise the risk if done over many years.
The inflammation caused by smoking doesn’t always appear immediately. In many cases, the pancreas may be slowly damaged for years before any symptoms develop. This is why many people are diagnosed with chronic pancreatitis only after significant, sometimes irreversible, tissue changes have already occurred.
Smoking After Diagnosis: Why It Makes Everything Worse
For those who already have pancreatitis, continuing to smoke can dramatically worsen the condition. Smoking not only slows recovery but also increases the frequency and severity of flare-ups.
Research has shown that smokers with chronic pancreatitis experience more pain and are more likely to develop pancreatic calcifications, where calcium deposits form inside the organ. These calcifications can block ducts and lead to digestive issues and malnutrition.
Additionally, smoking interferes with the body’s ability to absorb nutrients, which can worsen the nutrient deficiencies already common in pancreatitis patients.
And perhaps most concerning, smoking increases the risk of pancreatic cancer — a complication that can develop after years of chronic inflammation.
The Good News: Quitting Helps the Pancreas Heal
The pancreas is surprisingly resilient. Studies show that people who quit smoking can significantly lower their risk of developing pancreatitis — even if they’ve smoked for many years.
Within just a few weeks of quitting, blood flow to the pancreas begins to improve. Over time, oxidative stress decreases, enzyme function stabilizes, and inflammation subsides. While scarring or permanent damage may not fully reverse, stopping smoking can prevent further progression and improve overall digestive function.

Tips for Quitting Smoking If You Have Pancreatitis
Talk to your doctor – Medical professionals can offer personalized strategies and may recommend nicotine replacement therapy, patches, or medications to ease withdrawal.
Avoid alcohol – Combining alcohol and smoking increases stress on the pancreas. Stopping both can dramatically improve recovery.
Eat light, balanced meals – A low-fat diet with lean proteins, soups, and steamed vegetables helps reduce pancreatic load during the healing process.
Stay active – Gentle physical activity, like walking, can reduce stress hormones and help prevent cravings.
Find healthy distractions – Anxiety and restlessness are common during withdrawal. Meditation, breathing exercises, and hobbies can keep your mind occupied.
Seek support – Join online forums, support groups, or apps designed for people trying to quit. Accountability can make all the difference.
For those recovering from pancreatitis, the safest approach is complete nicotine cessation.
If you’ve been diagnosed with pancreatitis, quitting smoking is one of the most important steps you can take to protect your health and improve your quality of life. Every cigarette-free day allows your pancreas to function a little better — and your whole body to feel stronger.
Remember: healing from pancreatitis isn’t just about medication or diet. It’s about giving your body the chance to repair itself — and that starts the moment you stop lighting up.

