Periodontosis
Periodontosis is a chronic periodontal disease characterized by dystrophic changes in the tissues surrounding the tooth, without signs of inflammation. These changes lead to malfunction of the dental system.
Periodontosis is relatively rare. Although more than 60% of adults over 35 years suffer from various gum problems, periodontal disease occurs in only 2-4% of all periodontal diseases.
Signs and symptoms of periodontitis
In its early stages, periodontosis can be asymptomatic, making timely diagnosis difficult. The first signs of illness, such as pain, burning, and discomfort, usually appear late.
The main manifestations of periodontitis include
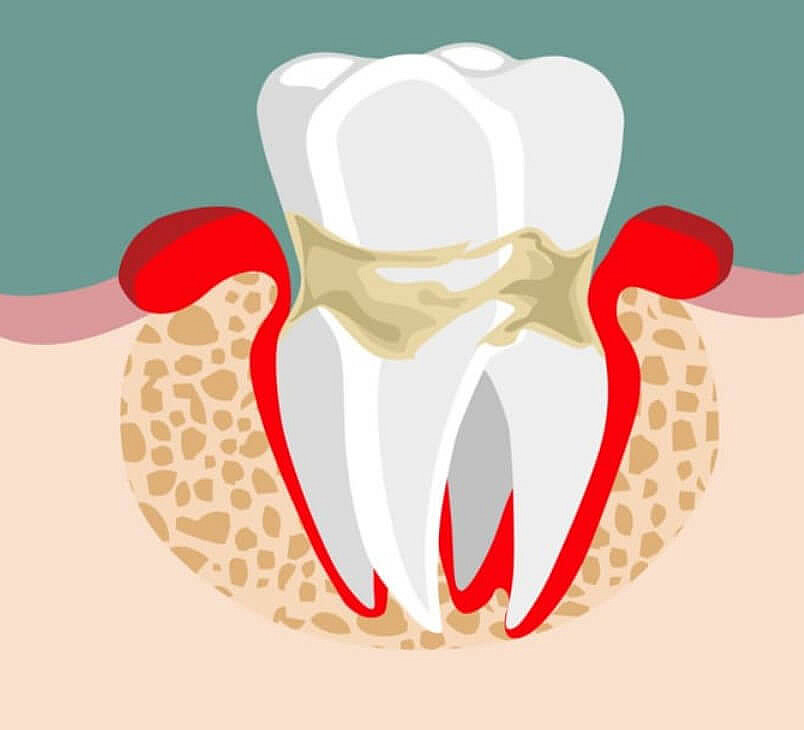
Gum drooping. This process can take years, leading to the exposure of the cervix.
Hypersensitivity of teeth. Bare teeth make the neck of the teeth more susceptible to cold and other irritants.
Bare root of the tooth. In some cases, a significant part of the root may be affected, and the tooth remains stable.
Gum discoloration. The gums may become pale or blue.
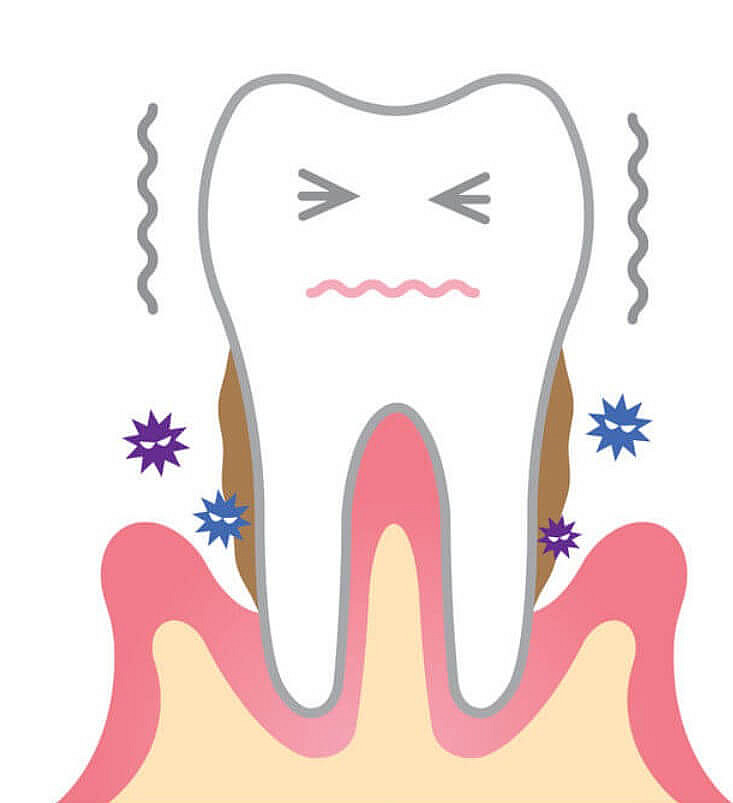
Periodontosis may be complicated by periodontitis, an inflammatory process that has its own characteristic symptoms:
Formation of deep gingival pockets.
Accumulation of bacteria and drainage of pus
Bad breath.
Mobility of teeth.
Gingival looseness.
Pain and discomfort.
Stages of periodontosis
Periodontitis can be acute, accompanied by symptoms of periodontitis, and chronic, characterized by slow, progressive tissue destruction. The chronic form is more common.
Lesions may be limited (involving a small area of the jaw including a few teeth) or generalized (affecting all of the bones in the jaw).
Periodontosis develops over several years and passes through several stages, each of which reflects the severity of the disease:
Initial stage: changes in periodontal tissues are invisible to the patient and can only be detected by the dentist during a thorough examination.
First stage: The gum begins to descend, but sensitivity of the teeth may be absent.
Second stage: Dystrophic changes become more pronounced, hyperesthesia (increased sensitivity of the teeth) occurs, patients may experience itching and burning in the gums. Sometimes there is a subjective sensation of tooth movement. The interdental spaces become noticeable, allowing food debris to accumulate and inflammation to develop.
Third and fourth stages: these are more severe forms of the disease, in which the roots of the teeth are exposed by more than 50-65%. The gaps between the teeth become more pronounced. Although there is significant tooth decay, there is no mobility, but eating is difficult due to fan-like tooth decay. In some people, teeth may change position.
Periodontosis is a complex systemic disease whose causes are not fully understood. There are several theories covering various aspects of its development, and many of them are supported by scientific research.
Atherosclerosis: Current studies, such as one published in Pharmacotherapy in 2000, suggest that atherosclerosis can impair bone nutrition, triggering dystrophic tissue changes and contributing to disease progression.
Local factors in the mouth:
Malocclusion: Incorrect tooth ratios can cause localized pressure, resulting in pathological changes.
Microbiome: Some bacteria cause inflammation, whereas others may contribute to dystrophic processes.
Prolonged tooth loss (adentia): This condition leads to malocclusion and bone destruction. The longer teeth are missing, the more severe the changes are in bone structure.
Diabetes mellitus: Studies emphasize a bidirectional relationship between diabetes mellitus and periodontal disease—one disease may exacerbate another.
Smoking: It is associated with the development of atherosclerotic diseases. For example, a study published in Odontology in 2004 found that smokers are more likely to suffer from periodontitis and periodontitis than non-smokers.
Osteoporosis and chronic stress: Both of these factors are also considered to predispose to periodontal disease.
Treatment of Periodontosis
Periodontosis is a chronic disease that cannot be completely cured, but it is possible to achieve sustained remission and slow the progression of dystrophic changes. The main goal of treatment is to eliminate symptoms, improve the condition of periodontal tissues and prevent further destruction.
Dental treatment algorithm
Oral health:
- Treatment of carious teeth and other dental diseases.
- Assessment of the condition of fillings, crowns and prostheses.
Professional oral hygiene:
- Removal of plaque, which is one of the causes of inflammation of the gums.
Hyperesthesia treatment:
- Remineralization of enamel for strengthening teeth.
- Surgery if necessary.
Surgical treatment
Which surgical treatment is used depends on the severity of the disorder. For mild periodontitis, patchwork surgery to close the gingival recessions may be used. However, eliminating the cause is important to achieve long-term results.
Marked changes in bone and dystrophic processes may require bone "building up". Bone grafts from the donor or the person themselves and materials that stimulate bone regeneration are used.
Restoration of lost teeth is also an important stage of treatment.
Physiotherapy and additional methods
Physiotherapeutic procedures are prescribed to improve blood circulation in periodontal tissues and accelerate the healing process. Gum massage and special exercises help to normalize blood circulation and improve the general condition of tissues.
A comprehensive approach to the treatment of periodontosis allows to achieve a significant improvement in the oral cavity and improve the quality of life of the patient.

